Access to gender affirming medical services differs from region to region. Healthcare workers say that's harming trans and gender diverse New Zealanders.
Warning: this article contains discussion of sexual violence and other content that may be distressing.
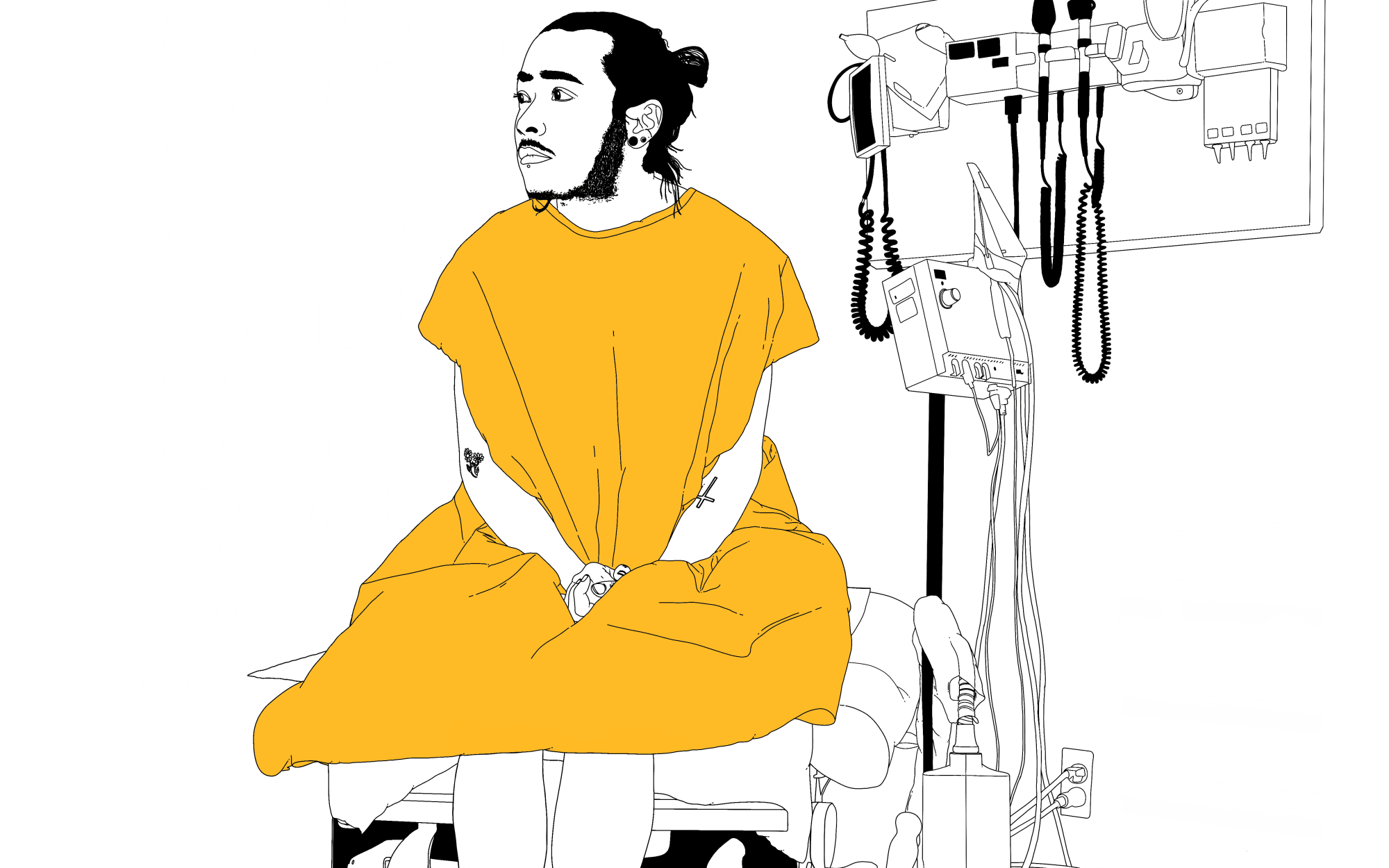
Krystal* looks around the dorm for the last time, wraps her belongings in a towel and makes her way to the office. There, away from prying eyes, she folds a pair of camouflage pants, packs her things and puts her shoes in a bag, the dirt still fresh. The others won't know she's gone until she's home.
The basic military training and life skills education course run by the Defence Force was supposed to be six weeks long, but four weeks in, Krystal has had enough. At 20 years old, this is not where she wants to be, but it's the path Work and Income and her GP thought would be best for her.
'It'll bring stability to your life', they told her, 'help you find out who you want to be'.
But Krystal doesn't need a course to figure things out. She's always known who she is and who she wants to be - in fact, all she wants is to start taking the hormones she's been asking for consistently over the past three years.
"I feel like I'm being pushed around. I feel like I'm asking for help and then they're putting me through this program, or another program or a counsellor," she says.
Years ago Krystal sat across from a counsellor and disclosed she was trans in the hope of accessing gender affirming healthcare. Instead, she was sent to a rape and abuse support service that works with victims in the Southland region.
She says it wasn't the only time healthcare providers tried to link her gender identity and poor mental health to being sexually abused as a child.
"They're like, 'Is this because of what happened years ago?' And I've tried to tell them, 'No it's not. It's got nothing to do with that. It's just the way that I am'," Krystal says.
Withholding or delaying gender affirming treatment in this way can cause harm by exacerbating any gender dysphoria (the feeling of discomfort or distress that can occur in people whose gender identity differs from their sex assigned at birth) or mental health problems, New Zealand's 2018 guidelines for gender affirming healthcare say.
"This is no different from harm that can be caused by withholding or delaying other medically necessary care".
The Professional Association for Transgender Health Aotearoa (PATHA) calls gender affirming healthcare "a medical necessity" and says inconsistent access to it is "an aspect of discrimination", which is causing harm.
Yet the inconsistencies across New Zealand's 20 district health boards (DHBs) are stark. In one area, a person's GP may be able to prescribe hormones, but if that same person was to live elsewhere, they might have to wait months to visit an endocrinologist who specialises in hormone treatment first. In other places, a psychological assessment and a formal diagnosis of gender dysphoria may be required before any medical intervention can take place. Across the country, the actual services provided can differ too: A person living in Whangarei may have access to a procedure or treatment that someone in Whanganui does not.
These inconsistencies have been described as "a postcode lottery" and the consequences can be lethal. According to 2018 survey Counting Ourselves, trans and non-binary people are nine times more likely to report high or very high psychological distress compared to the general population.
PATHA says pathways need to be streamlined and timely access to healthcare based on informed consent and self-determination needs to be provided.
*
Krystal grew up in the deep south, where ice-cold rivers flow across fertile plains into the Great Southern Basin and farmers reign supreme.
She says she struggled to be accepted as a teen - her school demanded to see proof of a gender dysphoria diagnosis before allowing her to wear makeup like the other girls. At 14, when she started dating another student - a boy - she says she was sent to a school counsellor and then to a priest. The relationship was viewed as gay. "I was made to feel like I had committed the biggest sin in the world. And I confessed my sins with the church and everything like that. Still, it makes me feel like I'm the problem." (The school's current principal, who has been there a year, says she has no knowledge of Krystal's complaint. The school's current pastoral care policies are "inclusive of all genders and identities", she says.)
Six years later, the country is about to go into Covid-19 lockdown. Krystal is sitting across from her GP in a small examination room. The kink that stayed in her hair long after she untied the bun she wore during military drills has finally relaxed. It feels like it took forever. She's mad that she was sent to do the training in the first place. "Look, I'm honestly sick of this," she says to her doctor.
Krystal's been with this GP her whole life - he knows more about her than any other medical professional. He wants to help but he doesn't have knowledge of trans healthcare, Krystal says. "He only knows as much as I tell him, and I only know as much as I can find out."
"He only knows as much as I tell him, and I only know as much as I can find out."
A lack of knowledge among health practitioners is a major barrier to accessing gender affirming healthcare; Counting Ourselves found that 46 percent of trans and non-binary people in New Zealand say they've had to teach a medical professional about their gender identity so they could get appropriate care.
And with differing pathways from region to region, it can be hard for both trans people and their primary healthcare providers to navigate the system.
PATHA founding president and psychology academic Dr Jaimie Veale says this needs to change. "It's very important that there's a national strategy on transgender health, which would aim to improve access to gender affirming health care, but also to ensure that the wider healthcare system is more competent in terms of being able to provide care in a way that meets the needs of trans and non binary communities," she says.
At present, though, a national strategy does not exist. There is no national coordination of gender affirming healthcare, no single source that patients or their healthcare providers can go to for information about what they're entitled to, or the process they must follow to get it. Instead, it varies from DHB to DHB.
Back in 2008, the Human Rights Commission reported that inconsistencies between DHBs meant it was rare for trans people to know what healthcare services were available. The report described a "paucity of information" and the absence of clear pathways as being barriers for trans people that could compromise their health.
At the time, the Ministry of Health indicated it would support the development of a treatment pathway that addressed the continuum of care from primary to specialist services. Twelve years later, that pathway still doesn't exist.
In 2018, PATHA recommended DHBs provide clear information about pathways to access gender affirming healthcare services. But currently that information - with the exception of the Hauora Tāhine service in Auckland - is not readily available.
That paucity of information is not the only barrier that trans people like Krystal face when trying to access healthcare.
Despite not having any gender affirming medical interventions, Krystal says her parents told her GP she was moving too fast with her transition. She never felt supported by them, she says. "My parents left me years ago, honestly, I felt so lonely, I felt like it's just been me in this world, I felt neglected hard out."
'Gatekeeping' is what Dr Jaimie Veale calls the high hoops some healthcare providers put in place for trans people to access the care they need. She says it comes from a history of viewing trans identities as mental illness, rather than viewing people as the experts of their own gender. But not allowing a person to be who they are comes with consequences. "We know that those who are experiencing barriers are more likely to experience mental health issues."
Within the Southern DHB catchment, it is a person's GP who provides referrals to different specialists - including psychologists and endocrinologists - who can help provide gender affirming healthcare.
Without her GP's support, Krystal can't get the care she needs. But she's determined. On that day in the doctor's office, fresh from the military training she never wanted, never asked for, she presents him with a plan. He finally refers her to an endocrinologist - a specialist who can prescribe the gender affirming hormones she so desperately needs. Krystal says she will travel to Dunedin to see the specialist - a four-hour round trip from her home.
This kind of travel is yet another barrier faced by many - especially those in small towns and rural areas, national coordinator of Gender Minorities Aotearoa Ahi Wi-Hongi says.
"In some cases, there might not be a GP in the area, or there might be only one in the area. And that could be your family GP and perhaps you don't want family to know about what's happening. Or it could be that the GP isn't very supportive. There are many reasons why it might be difficult," Wi-Hongi says.
And for people on lower incomes, trips to bigger centres to access specialist care can be out of reach. "We know that it's very likely that trans people are on low income, or don't have any income, which makes it more likely that they don't own a car or they don't have the luxury of being very mobile.
"You might be living at the very bottom of the South Island and the endocrinologist might be halfway up South Island. Then you go to see them and they require a psychologist... If that psychologist wants to see you six times, that's a huge amount of travel around the country disrupting your work, or your studies, or your whānau commitments. So it's a really, really high barrier to getting what should be basic health care that can be prescribed to you by your GP", Wi-Hongi says.
"People shouldn't be expected to take a bus for six or eight hours every time they need to get an appointment just to get their basic healthcare needs met".
But for Krystal, even getting to the point where she is referred to a specialist - regardless of where they are - has been a struggle. Without an advocate, she feels lost, overwhelmed and alone.
"There's not much help down here and it shows how much they don't want to help us", she says. Her voice grows tired. It's clear she is holding back tears as she describes being directed from one service to another, never seeming to get closer to her goal.
"My life's been incredibly hell. I don't know how I managed to live like this, but I have. I'm so, so lonely. And I don't blame anyone but myself, right?"
*
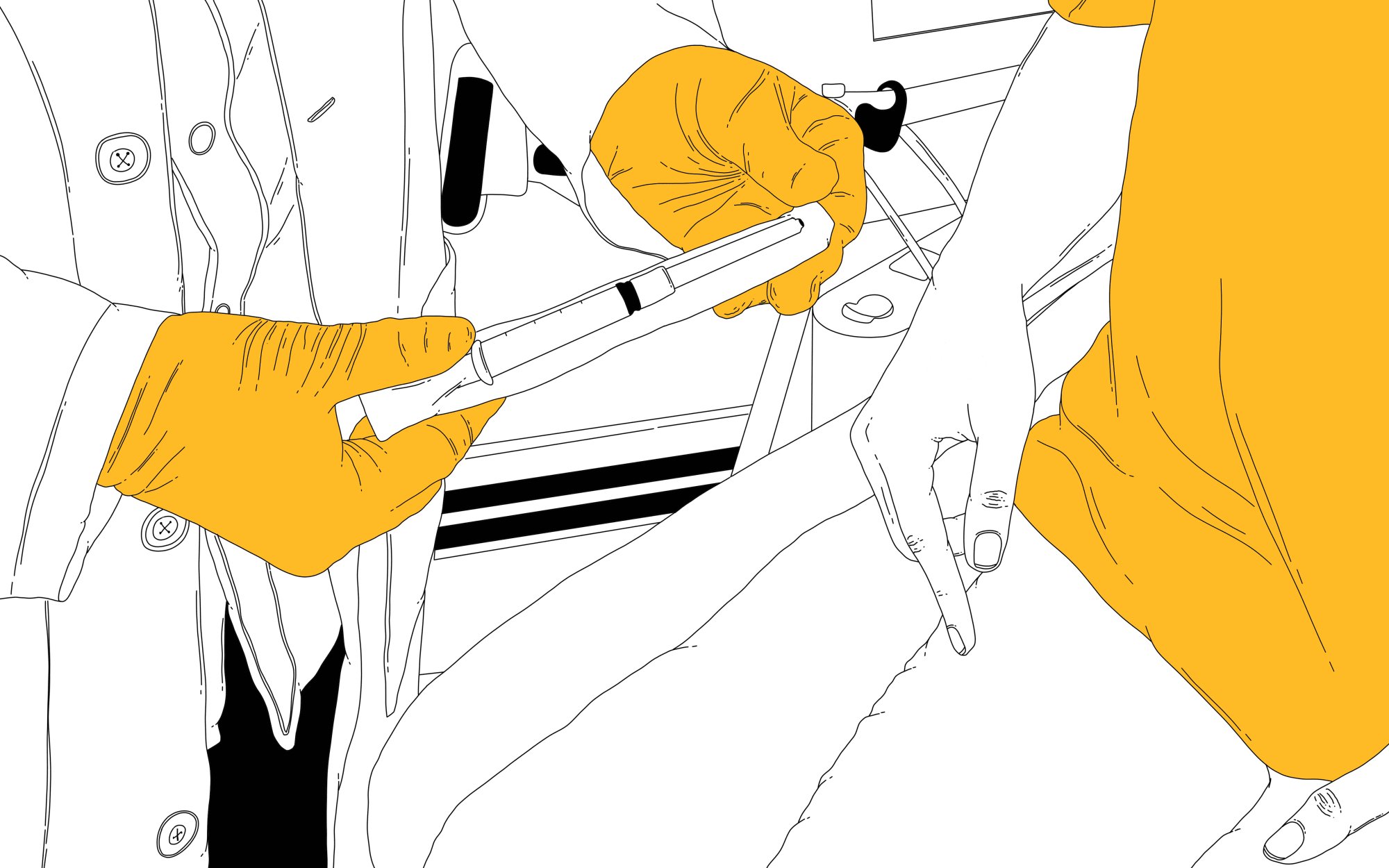
Photo: Huriana Kopeke-Te Aho / Gender Spectrum Collection / RNZ
As part of her 2020 thesis, Wellington psychologist Gloria Fraser spoke to 13 young adults about their experiences accessing gender affirming healthcare. Participants described its provision as a "postcode lottery" with care available being largely dependent on where people lived.
"Larger cities like Auckland and Wellington were generally described as easier places to access gender-affirming healthcare than smaller cities, towns, or rural areas," Fraser says.
Participants of her study also described waits for publicly funded psychology assessments (which, within many DHBs, is a requirement before hormones can be prescribed) being so long that it was routine to pay to see a private practitioner instead.
Fraser says these barriers have significant implications for the health and wellbeing of trans New Zealanders, and show the urgent need for increased funding for trans healthcare.
Leo* knows only too well about assessments, long waits and trips out of town to get the care they need.
Not long ago, they were finally offered the job they'd been looking for - one that would get them off minimum wage. But taking the job was a double-edged sword. Financial stability was good, but it meant a move from Christchurch to Nelson; Leo's new life in a new city would mean finding a new, trans-friendly GP, within a new DHB catchment.
Leo had to forfeit their place on the Canterbury waiting list to see a psychiatrist and start the whole process again, navigating a new, different pathway within the Nelson Marlborough DHB in order to get the care they need. They just want to start on hormones.
"That was a pretty disheartening time, honestly, for me in terms of gender dysphoria and transition, because I realised that I was going to have to go through the whole process again".
To get on hormones within the new DHB, Leo first needs a diagnosis of gender dysphoria from a psychologist, who will then provide a referral to see an endocrinologist at Nelson hospital. But there is no public funding for the psychological assessment required - Leo will need to pay to see a private practitioner. On top of this, Leo's GP says there are no psychologists in Nelson with the expertise required to make the assessment. Leo will need to make a three hour-plus round trip to Blenheim.
Though not the case everywhere, within the Nelson Marlborough DHB area, a diagnosis of gender dysphoria is a requirement for anyone wanting to start taking gender affirming hormones. (For people in the region who are 21 and under, only six psychological assessments are publicly funded, so going private is the most common option anyway.)
Dr Jaimie Veale says the requirement for a diagnosis of gender dysphoria before any medical intervention can take place is yet another barrier placed between trans people and the healthcare they need, but it shouldn't be. "It's not requirement as part of the latest The World Professional Association for Transgender Health (WPATH) or the the Aotearoa New Zealand Guidelines for Gender Affirming Healthcare which are endorsed by PATHA".
Veale says requiring a formal diagnosis pathologises trans identities - treating people as abnormal, or as having an illness. But she says it's important trans people are able to make informed choices for themselves, rather than coming up against barriers again and again. It's also important to note, she says, that not all trans people experience gender dysphoria. But without it, they should still be able to access care.
"It makes me feel like being trans is some medical fault that needs fixing," says Leo. "It makes me feel like I need this person to validate or improve my transition - [like] my understanding of my own gender isn't enough."
"It makes me feel like being trans is some medical fault that needs fixing"
Leo is non-binary - they don't identify as male or female. But they seriously considered telling medical professionals they were a trans guy in order to have their identity treated more seriously and to access the healthcare they were seeking faster. They felt pressured to appear more masculine too.
"Like the idea that if you don't present in a way that's consistent with the gender that you say you are, then you're less likely to be taken seriously, or people will think you need access to healthcare less.
"I didn't do that and I'm glad I didn't do that, because it would have felt kind of shitty just misgendering myself to my healthcare provider."
*
Sitting in a suburban Christchurch doctor's office on a comfy chair, surrounded by posters offering advice about staying healthy, Jennifer Middendorf's GP scrolls through the Canterbury DHB website looking for pathways to access publicly funded chest reconstruction surgery - also known as a subcutaneous mastectomy, or top surgery. From over his shoulder Middendorf reads the notes - the pathway requires them to first be on hormones. But Middendorf didn't want to take hormones.
"So for a start, that pathway just wasn't going to fit me", Middendorf says, recalling how the experience made them feel. Earlier, they had disclosed they were trans non-binary to the GP. "His first question was, 'What does non-binary mean?'"
The GP found Middendorf a psychologist with knowledge of trans healthcare. But the psychologist hadn't heard of anyone in Canterbury getting chest reconstruction surgery without first going on hormones.
Gender Minorities Aotearoa national coordinator Ahi Wi-hongi believes it's this type of requirement that pressures people into having unnecessary medical interventions.
Not wanting to go on hormones, the only other option for Middendorf was to go private. At 51, they recognise their privilege - they've got a good job, their family has money and they were able to cobble together the $18,000 needed to pay for top surgery.
Ten percent of trans or non-binary people have paid for chest reconstruction surgery, the Counting Ourselves survey found. But in 2019, almost half of all trans and non-binary people who wanted the surgery said they had an unmet need. Cost, alongside medical practitioner knowledge, was the biggest barrier they faced.
The surgeries that are available differ from region to region. Some DHBS offer gender affirming mastectomies, hysterectomies, orchiectomies (testicle removal) and breast augmentation, while others offer only some, or none.
Counting Ourselves found that of those who had accessed gender affirming care, one in ten have moved to another part of the country in order to get access to the service because it wasn't offered in the DHB region they were living in.
"I'm actually moving to Christchurch in April and I have to give up everything that I've got down here just for this transition, because there's no help down here," Krystal says. A sense of urgency increases her pace as she jumps from one topic to another and back again.
"I don't think [the DHB] understands how it feels. Because I feel like f***ing shit. And I'm not even gonna lie, like, there's been times where this has made me feel so dark..."
But, she says, "I'm one of those girls that doesn't give up...I'm gonna get this.
"I'm over my voice not being heard."
*
Additional reporting by Susan Strongman
*Names and some details have been changed
**Trans and non-binary are used in this article as umbrella terms for people whose gender/gender expression is different to their sex assigned at birth, while acknowledging that these are Pākehā terms that cannot fully describe the meaning of genders that come from other languages or cultures.
Where to get help:
If it is an emergency and you feel like you or someone else is at risk, call 111.
1737 - Need to Talk? Free call or text 1737 any time to speak to a trained counsellor, for any reason.
OUTline: 0800 OUTLINE (0800 688 5463) every evening, 6pm to 9pm.
Rainbow Youth: (09) 376 4155
Gender Minorities Aotearoa: 020 404 92568
Lifeline: 0800 543 354
Suicide Crisis Helpline: 0508 828 865 / 0508 TAUTOKO (24/7). This is a service for people who may be thinking about suicide, or those who are concerned about family or friends.
Depression Helpline: 0800 111 757 (24/7)
Samaritans: 0800 726 666 (24/7)
Youthline: 0800 376 633 (24/7) or free text 234 (8am-12am), or email talk@youthline.co.nz
What's Up: online chat (7pm-10pm) or 0800 WHATSUP / 0800 9428 787 children's helpline (1pm-10pm weekdays, 3pm-10pm weekends)
Kidsline (ages 5-18): 0800 543 754 (24/7)
*
This story is part of Here We Are, an RNZ series about transgender mental health. You can read, hear and view more stories at rnz.co.nz/here-we-are.
Here We Are was made with the help of the Mental Health Foundation and Like Minds, Like Mine